Telehealth Snapshot: Use Cases, Policies & Hybrid Care
At the Telehealth22 Virtual Summit, telehealth experts gathered to discuss virtual chronic disease management, the evolving hybrid care model, the regulatory landscape, and more.

Source: Adobe Stock
- As the COVID-19 pandemic hit, telehealth use skyrocketed, helping providers deliver quality healthcare when in-person services stalled. Though telehealth use has leveled off over the past year, providers and payers see the modality as a key part of care delivery moving forward.
Speakers at Xtelligent Healthcare Media's Telehealth22 Virtual Summit, held in March, discussed a wide range of issues related to telehealth, including how telehealth can help improve chronic disease patient outcomes, the barriers standing in the way to patient access and provider adoption, the hybrid care model that is being developed, and the current regulatory landscape governing telehealth use.
ENHANCING CHRONIC DISEASE CARE
Telehealth has shown significant potential in improving chronic disease management as it enables clinicians to keep track of health metrics beyond in-person visits.
"We have seen a lot of examples where organizations are thinking about how they can use telehealth to really do even better in their care quality than they were doing before the pandemic," said Kate Kirley, MD, director of chronic disease prevention and programs at the American Medical Association, during a panel discussion. "They're looking for new opportunities. They're not just thinking about this as implementing in-person care virtually."
Hypertension, diabetes, and chronic heart conditions are some diseases that health systems are treating virtually.
For example, the American Medical Association collaborated with federally qualified health centers and the National Association of Community Health Centers on a project that aimed to improve statin use among high-risk patients. The project focused on helping health centers implement brief counseling visits with their patients to address care gaps.
"And they're seeing some really great movement in improving their care quality by using telehealth to augment their in-person care," Kirley said.
The University of Alabama at Birmingham Health System is using telehealth in various clinical scenarios, including critical care, stroke, and nephrology, said Eric Wallace, MD, the health system's director of telemedicine, director of the UAB Home Dialysis Program, and co-director of the UAB Fabry Disease Clinic, during a panel.
To support its telehealth-enabled chronic disease care programs, UAB Health System deployed and scaled e-consults. This allows the system to keep an eye on its patients between clinic visits in a convenient way for all parties.
"I think that long term, that's great for the patients, it's great for the rural hospitals, it's great for the tertiary referral centers," said Wallace. "So, we can open up access for really the sickest of the sick."
This includes cancer patients. When the COVID-19 pandemic hit, cancer care went into a tailspin as these patients were at high risk for contracting the novel coronavirus. As a result, health systems had to make cancer care virtual.

Source: Xtelligent Healthcare Media
Kaiser Permanente went from 15 percent of its cancer care visits being conducted virtually to 98 percent in one week, said Tatjana Kolevska, MD, chair of medical oncology and hematology at the Permanente Medical Group and medical director of the Kaiser Permanente National Cancer Excellence Program, at a panel discussion.
Virtual cancer care involves patients attending clinic visits and follow-up appointments remotely. If they require treatment, like chemotherapy, the physician can order the treatment, and patients can go to a local center to receive it, Kolevska explained. Virtual cancer care has stabilized at about 60 to 70 percent of all visits at Kaiser Permanente.
The health system found that physicians, patients, and families were satisfied with cancer care delivered via telehealth.
"It was quite interesting that even when patients were discussing challenging diagnoses with doctors, they were actually very happy that they could do a video consultation where all their family members from across the world can sign in, and the whole family can actually be together," said Kolevska. "So that was a huge advantage."
Another way in which telehealth can help address chronic care needs is by offsetting the shortage of primary care physicians, particularly in rural areas.
"Good outpatient [primary] care can prevent complications, can delay the onset of complications, and have a very high impact on the management and maintenance of chronic diseases," said Saurabh Chandra, MBBS, PhD, chief telehealth officer at the University of Mississippi Medical Center's Center for Telehealth, during a panel. "So, if you don't have enough primary care physicians, then what does the patient do? They go to the nearest emergency department, they go and get admitted to the hospital, which drives [up the] overall cost of care, depleting the resources."
Telehealth can bring primary care to the patient, no matter how far they live from a healthcare facility, enabling more comprehensive management of their chronic conditions.
The University of Mississippi Medical Center, which serves a largely rural population, uses remote patient monitoring and telehealth to manage diabetes, among other chronic diseases. A remote team of physicians and nurses gather blood glucose readings for diabetic patients every day and use that information to educate the patient and adjust their medications and treatment plans, Chandra said.
Not only does telehealth offset primary care physician shortages, but it also widens access to specialty care. Kaiser Permanente is building a virtual center of excellence for cancer care, where experts in various cancer types can consult with local physicians across the country.
"No matter where the patient lives — they can live in a small village in Hawaii — because we have Kaiser Permanente in Hawaii, they actually all have access to all our experts," Kolevska said.
ADDRESSING BEHAVIORAL HEALTH CONDITIONS VIRTUALLY
During the COVID-19 pandemic, the need for behavioral healthcare skyrocketed, resulting in a massive spike in telemental healthcare use. In a recent survey, about 17 percent of respondents said they used virtual mental health services in 2021, compared with 11 percent in 2020.
Even among older adults, tele-behavioral healthcare use shot up, with Medicare beneficiaries receiving 14.1 million behavioral health services virtually in 2020, including individual therapy and substance use disorder treatment.
But specialists, especially those providing mental health services, tend to live in areas where other people live, said Taft Parsons III, MD, Humana's enterprise medical director for behavioral health, during a panel.
This is where telehealth can help.
"It doesn't matter where the clinician is, as long as they have the appropriate licensure, they can practice in multiple different locations," said Parsons. "And so, [telehealth] does help to spread out the [behavioral health] providers that are there."
Telehealth has proved to be a preferred mode of care delivery for behavioral health patients.
Even as COVID-19 cases ebbed and in-person care returned, a significant portion of Humana members have continued with virtual behavioral healthcare, Parsons said.
"And we saw that in our provider network as well," he added. "A lot of therapists and psychiatrists figured out that they actually liked the convenience of working from home, not spending a lot of time driving in the car doing what we call windshield time, which is just non-productive time that you can't see patients."
Humana is conducting pilots with different vendors to offer virtual care solutions to its members. One pilot involves passively monitoring severely mentally ill members via an app on their phone, Parsons said. The app alerts providers to the members' needs based on algorithms developed by the passive monitoring, allowing providers to deliver wraparound care.

Source: Xtelligent Healthcare Media
The University of Texas Health Science Center at Houston (UTHealth) is focusing on providing tele-behavioral care to vulnerable populations across the state of Texas, said Jane Hamilton, PhD, assistant professor of psychiatry and behavioral sciences and director of the Mental Health Services and Outcomes Research Program at UTHealth, during a panel discussion.
Through a grant provided by the Substance Abuse and Mental Health Services Administration, UTHealth is leveraging telehealth to deliver mental healthcare to the homeless population in shelters and those living in encampments.
Further, UTHealth is using Project ECHO, a collaborative medical education and care management model, to provide virtual training on mental healthcare interventions to local providers.
BARRIERS TO TELEHEALTH USE AND STRATEGIES FOR SUCCESS
Inequitable access to the technologies needed for telehealth services is one of the most intractable barriers to virtual care.
"Telehealth represents an immense opportunity to connect patients who have been disconnected from the healthcare system," AMA's Kirley said. "But we need the tech to do that. We need broadband access to do that…So, there's a lot of pieces that need to come together."
Though these issues cannot be solved by healthcare stakeholders alone — broadband access requires investment from the government, for example — there are some pieces in providers' hands, including digital health literacy.
Patients must be taught how to use the devices that enable virtual care. Otherwise, the data collected will be inaccurate, Kirley said.
"So, you either need to have a solution that's really well designed and will educate and onboard that patient," she added. "Or you need a person; you need a human to do that."
If care team members are tasked with patient education and onboarding, they need to be trained as well.
The technology access issue is magnified among vulnerable populations. For example, a significant barrier to UTHealth's efforts to bring teletherapy to the homeless was that many did not have cell phones, which is why they had to provide the patients with phones funded through grants.
"We obtained a pilot residency training grant from the American Psychiatric Association to provide cell phones for the homeless, as well as low-cost cell services that we pay for through the grant," said UTHealth's Hamilton.
UTHealth then developed strategies to combat the lack of digital literacy. UTHealth workers assess a patient's capacity to conduct a video visit or use an app during their first therapy session and train them if needed. They also ensure patients can test their devices before their scheduled teletherapy appointment and train all staff, including the therapists, to troubleshoot technology issues.
Another strategy to prevent technology access issues is to set up telehealth hubs and external sites where patients can go for virtual visits.
"The patient just goes in, sits down, and then does a connected visit where they are not responsible for the tech — [that] is probably the truest way to make sure that everybody has options," UAB Health System's Wallace said.
Then there is the issue of the technical infrastructure for virtual care, which needs to be updated to ensure interoperability, according to Wallace.
For example, e-consults require physicians to have access to medical records. Currently, providers must rely on getting the EMR data through health information exchanges.
"And I think our current exchanges leave a lot to be desired, but access to information across the entire country is really what's necessary to facilitate this," Wallace said.
Chandra echoed this, adding, "We have to deal with getting the right kind of data coming to us and then sending back the data; I think it's imperative that we should have some kind of [interoperable] mechanism for exchanging data."
Lack of insurance coverage further erects barriers to virtual care, Chandra said. Though there are currently several waivers and temporary coverage rules that enable public and private insurers to extend access to telehealth, most will end a few months after the public health emergency is declared over.
Healthcare stakeholders have made a concerted push to make these temporary flexibilities permanent. Further, several bills that do just that are winding their way through Congress.
Along with solving issues related to regulatory flexibilities, technology access and use, and data sharing, providers must continue to enhance their digital front door to break down virtual care barriers. This will enable patients to avail themselves of the virtual care options that providers offer.
"We're really looking to innovate that interaction with patients so that it's as easy to book an appointment, or pay for care, or even get care virtually, as it is for you to transfer money in a bank account," said Adam Hornung, executive director of telehealth operations at Intermountain Healthcare, during a panel.
Intermountain is focusing on making digital access to care informative, easy, and customized to each patient's preference. For instance, some patients may prefer to receive notifications from their providers on a device, and others may prefer to communicate via email or traditional mail.
"I think it's on us as an industry to make sure that we create as many easy front doors as possible," Hornung said. "And if we can do that, we're going to reach a lot more people than we are currently. And I think that's kind of the hunt for everybody right now — how do you make it easier for people to get what they need as fast as they need it?"
CREATING A HYBRID MODEL OF CARE
As the COVID-19 pandemic ebbed and surged, so did the volume of care delivered via telehealth.
During the early stages of the pandemic, telehealth use rose to 13 percent of outpatient visits, followed by a drop to 8 percent in 2021, according to data from the Peterson- KFF Health System Tracker. But patients have indicated that they want to continue using telehealth alongside in-person care, which means health systems will have to develop a hybrid model of care with various digital touchpoints.
"As we think about telehealth 2.0 — it's not just telehealth only, but it's really a digitally enabled system of care," said Kristi Henderson, DNP, CEO of Optum Everycare, in a keynote address. "It really allows us to start thinking about new ways to treat healthcare as a distribution model to get the right resources to the right place at the right time."
Adding digital resources like symptom checkers, online scheduling, and the option for virtual visits can all help medical practices improve their operational efficiency.
"Really, if we think about it as a fibrous network connecting the system of care, there's a lot of digital support services that can support a practice," she said.
For instance, online scheduling gives people a great deal of flexibility. When they are off from work and not busy, they can schedule an appointment online and add it to their calendar, she explained. When the time comes, they can click on their appointment from their calendar and jump into a video visit or interact with their care team through chat.
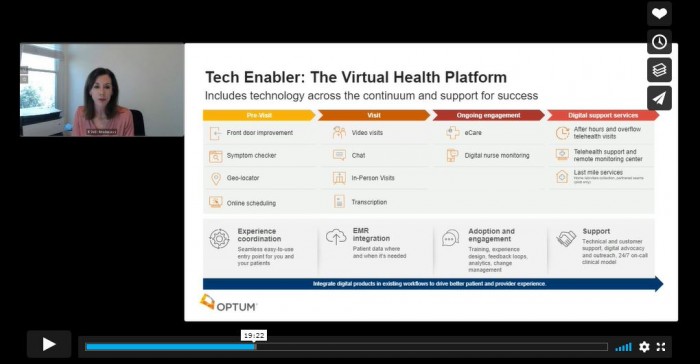
Digital tools can also help personalize care by matching patients to a provider that can meet their care needs, whether male or female, a particular ethnicity, or a speaker of a specific language.
In a hybrid model of care, digitally enabled care delivery will also allow patients to move easily between in-person care and telehealth.
Patients can begin their care journey by scheduling a virtual visit, then come into a facility to get their blood drawn for lab work or get a vaccine shot, and then have a virtual follow-up visit with their provider.
"It's exciting to think about the possibilities there," said Henderson. "It's very broad and can be daunting, but if we think about the pain point and the friction point for both our patients and our providers and the clinical team, then you'll see the places where we have amazing opportunities to optimize how we use technology."
NAVIGATING THE REGULATORY LANDSCAPE
As providers fine-tune their existing telehealth processes and work to integrate them seamlessly into traditional care delivery, federal and state policymakers are debating the regulatory framework needed to support this brave new world of healthcare.
Last month, Congress passed a new omnibus spending bill that extended certain telehealth flexibilities for Medicare patients for at least five months after the public health emergency officially expires. These include a waiver that removed geographic requirements and expanded originating sites for telehealth services and one that struck down the requirement that mental health patients had to meet a provider in-person before receiving care virtually.
The American Telemedicine Association, whose advocacy arm is working to move the needle on telehealth policy in Washington, aims to make many of these flexibilities permanent.
"Years of literature…show that telehealth is a clinically appropriate modality of care in a variety of situations [and] the standard of care that is laid out for in-person care, of course, applies to virtual care services," said Kyle Zebley, vice president of public policy at the American Telemedicine Association, and executive director of ATA Action, in a keynote address. "And all we are asking is that our licensed medical professionals…are able to determine the appropriate method of delivering care."
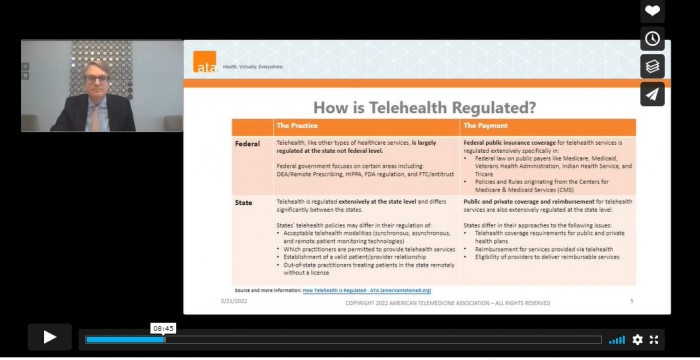
In addition to solidifying flexibilities extended by the omnibus spending package, ATA Action seeks to make permanent a tax provision that allows for first-dollar coverage of telehealth for high deductible health plans and a waiver that enables providers to prescribe certain controlled substances virtually.
Since the beginning of the pandemic, states have also passed bills expanding access to telehealth and loosening restrictions on adoption en masse.
"2021 was the most successful year in the history of state telehealth policy," Zebley said.
But there are still concerns about telehealth use that hamper efforts to get legislation passed.
"There's this idea out there that somehow telehealth might be more prone to fraud, waste, and abuse," Zebley said. "That somehow telehealth might be a cost driver because of potential concerns of overutilization."
But telehealth is no more prone to fraud, waste, and abuse than in-person care, according to Zebley. Telehealth even includes a digital trail that helps ensure accountability for reimbursement.
Further, telehealth can help increase access to preventive care, ultimately driving down healthcare costs.
"Many of these concerns are unfounded," Zebley said. "All we're asking for is that telehealth should be held to the same standard as in-person care, that we empower our medical professionals, that we don't slice or dice those services or those modalities…And that we continue to ensure that telehealth is an option and a tool to reduce [health] inequities."
To learn more about Xtelligent Healthcare Media virtual summits, visit our event page.
