The highly competitive digital healthcare market is teeming with companies looking to achieve a singular goal: create solutions with staying power. In recent years, companies have launched and folded in short order, showing that developing effective digital health tools is a formidable task. As...
[RevCycleIntelligence]

Pandemic volume changes underscore rural hospital concerns
[HealthITSecurity]

Insider threats in healthcare remain prevalent
[PharmaNewsIntelligence]

Healthcare Realty Trust, KKR forge medical outpatient JV
[LifeSciencesIntelligence]
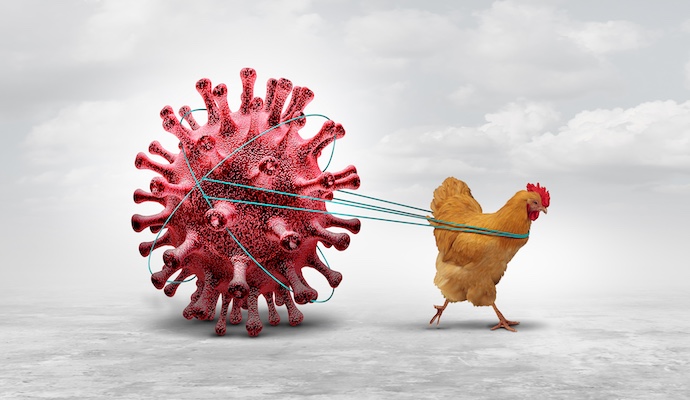
Caution urged as bird flu spreads among cattle and dairy workers
Do Not Sell or Share My Personal Information
©2012-2024 TechTarget, Inc. Xtelligent Healthcare Media is a division of TechTarget. All rights reserved. HealthITAnalytics.com is published by Xtelligent Healthcare Media a division of TechTarget.