Hospice plays a critical role in providing care and comfort to patients at the end of their life. A challenging time for patients and their loved ones, hospice care relies on coordinated efforts from various experts, including physicians, nurses, social workers, and spiritual advisors, according...
[LifeSciencesIntelligence]

Ultrahuman launches US-based wearable ring manufacturing facility
[HealthPayerIntelligence]

Humana reports Medicare Advantage growth, income gains in Q1 2024
[HealthITAnalytics]
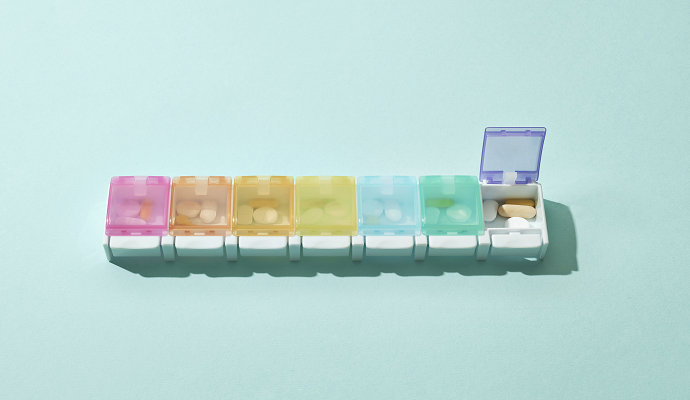
LLMs may enhance geriatric polypharmacy management in primary care
Do Not Sell or Share My Personal Information
©2012-2024 TechTarget, Inc. Xtelligent Healthcare Media is a division of TechTarget. All rights reserved. HealthITAnalytics.com is published by Xtelligent Healthcare Media a division of TechTarget.